Retreatment CasesCase 1After RCT was completed, the final PA radiograph revealed canal bifurcation at the apical 1/3.   Case 255 YO Caucasian female, denied of any significant medical history. Presented to clinic with localized buccal swelling in the #21 area. Noted also facial vestibular swelling. Dx was acute apical abscess secondary to non-healing previous endodontic treatment of #21. 1 Pre-op radiograph was taken and a CBCT scan was performed.    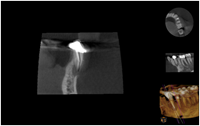  Case 340 YO South East Asian healthy male self-referred to our office for #18 and19. RCT for #18 and 19 had been completed not long before, however, both teeth remained symptomatic; there was percussion and biting pain for both #18 and 19. Probings were normal and slight palpation discomfort. Both accesses were sealed with amalgam. Pre-op radiograph showed under-prepared and obturated #19 and under-prepared and overextended #18. Apical RLs noted for both #18 and 19. Non-surgical retreatment was recommended for both.   Upon access, I noted Thermofil was used for obturation material. There were all removed, all canals were cleaned, shaped, and then obturated. #18 displayed C shaped anatomy.  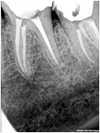 Case 4Silver point retreatment. 59 YO Caucasian male with a medical history of hypertension and adult onset type 2 diabetes. No known drug allergies. He presented to clinic with acute apical abscess of #31. Noted submandibular swelling and vestibular space abscess. Tooth #31 was painful to percussion, and palpation. Probings were WNL. Non-surgical retreatment and I+D were recommended and patient consented. Pre-Op Access was made through the PFM. Located silver points in the MB and ML canals. Distal canal was previously obturated with gutta percha. All canals were then cleaned, shaped, and irrigated with NaOCl and EDTA. Canals were then medicated with Ca(OH)2 and temporized.   |